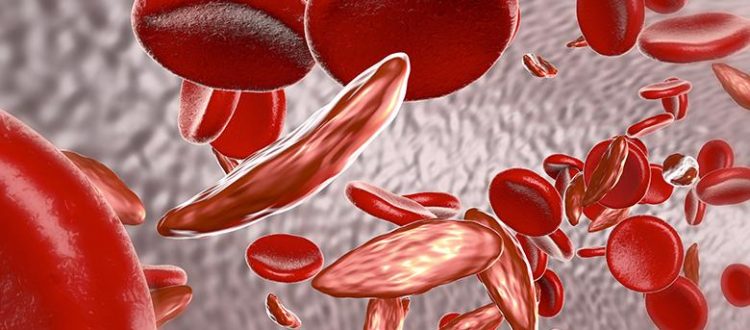
Sickle cell nursing workforce project: Overview and call for evidence
Introduction and background:
One of the clear findings of the sickle cell care inquiry conducted by the Sickle Cell Society and the APPG on Sickle Cell and Thalassaemia, as detailed in the ‘No One’s Listening’ report, was that inadequate staffing levels for sickle cell care are a key factor in the care failings sickle cell patients encounter. The inquiry was told of “chronic under-staffing”, with fears that the problem is on course to get worse without action, due to an ageing staff demographic and too few replacements.
The report also detailed evidence that the lack of specialist nurses for sickle cell care means that patients encounter healthcare professionals without the appropriate knowledge of their condition, which exacerbates issues around stigmatisation, lack of joined-up care and care failings.
The Sickle Cell Society is now undertaking a research project to gain a more detailed understanding of the current level of nurse staffing for sickle cell (and other rare anaemias), the impact this has on patients and clinicians, and what needs to happen to ensure there are sufficient numbers of nurses to deliver a good standard of care to people with sickle cell disorder.
What the research project aims to explore:
The Sickle Cell Society would welcome evidence from a range of individuals and organisations, such as individuals with sickle cell disorder, family members and carers of people with sickle cell disorder, healthcare professionals, healthcare bodies and other relevant organisations. We have suggested below questions that may be most relevant to different respondents but please feel free to answer any questions you wish to respond to:
For patients and carers
- In your experience, is there generally a sufficient number of nurses to provide a good standard of sickle cell care?
- In your experience, is there a sufficient number of nurses who specialise in sickle cell?
- In your experience, how does the level of nurse staffing in the community compare with in-patient hospital settings?
- What is your impression of how the level of specialist nurse staffing for sickle cell compares with other conditions such as cystic fibrosis and haemophilia?
- What impact does the current level of nurse staffing have on your (or your loved one’s) care?
- What is your impression of the impact the current level of nurse staffing has on the nurses who deliver your (or your loved one’s) care?
- What do you (or your loved one) require from the nurses who care for you? What does good care and support look like?
For nurses and other healthcare professionals
- In your experience, is there generally a sufficient number of nurses to provide a good standard of sickle cell care?
- In your experience, is there a sufficient number of nurses who specialise in sickle cell?
- What factors affect how many nurses choose to specialise in sickle cell?
- To provide a good standard of care, what would you say the ratio should be of number of sickle cell patients per specialist nurse employed? What is the current ratio in your service?
- How does the level of nurse staffing in the community compare with in-patient settings?
- What is your assessment of the level of availability of nurse counselling for sickle cell patients?
- How does the level of nurse staffing for sickle cell compare with other conditions such as cystic fibrosis and haemophilia?
- How has the level of nurse staffing changed during the time you have been working? Is it better, the same or worse? What are the reasons for this? What impact did the pandemic have?
- What impact does the current level of nurse staffing have on you and your colleagues?
- What impact does the current level of nurse staffing have on sickle cell patients?
- If you believe the current level of nurse staffing for sickle cell is insufficient, what do you believe needs to happen to increase numbers? Are there steps other than increasing funding that need to be taken?
- What needs to happen to increase retention of the sickle cell nursing workforce?
- What is your expectation of what will happen to sickle cell nursing workforce levels in the coming years without a change of approach?
- Is regular training on sickle cell provided to nurses in your NHS Trust who are not specialists in sickle cell? If so, can you describe this training and its frequency?
- What does or what would a good training pathway to develop specialist sickle cell nurses look like?
- [If you work in the community] To what extent do you feel you have appropriate coordination with colleagues in secondary care?
- [If you work in secondary care] To what extent do you feel you have appropriate coordination with colleagues in community settings?
For healthcare bodies
- Is there generally a sufficient number of nurses to provide a good standard of sickle cell care in England?
- Is there a sufficient number of nurses who specialise in sickle cell?
- What factors affect how many nurses choose to specialise in sickle cell?
- Are there challenges in filling sickle cell nurse vacancies? If so, why is this?
- To provide a good standard of care, what should the ratio be of number of sickle cell patients per specialist nurse employed?
- How does the level of nurse staffing in the community compare with in-patient settings?
- What is your assessment of the level of availability of nurse counselling for sickle cell patients?
- How does the level of nurse staffing for sickle cell compare with other conditions such as cystic fibrosis and haemophilia?
- What impact has the pandemic had on the sickle cell nurse workforce?
- What impact does the current level of nurse staffing have on nurses and other clinicians?
- What impact does the current level of nurse staffing have on sickle cell patients?
- If you believe the current level of nurse staffing for sickle cell is insufficient, what do you believe needs to happen to increase numbers? Are there steps other than increasing funding that need to be taken?
- What needs to happen to increase retention of the sickle cell nursing workforce?
- What is your expectation of what will happen to sickle cell nursing workforce levels in the coming years without a change of approach?
The Sickle Cell Society will consider the evidence presented to it and present its recommendations in a report to be published in late 2023.
Submission guidelines:
Submissions of written evidence should follow the guidelines below:
- Be submitted as a Microsoft Word document
- State clearly who the submission is from, and whether it is sent in a personal capacity or on behalf of an organisation
- Be no more than 2,500 words in length
- Comprise a single document attachment to the email.
There is no requirement to answer every question above and respondents should feel free to choose the questions they can most usefully cover. Accounts of personal experience and anecdotal evidence is welcome. The Sickle Cell Society would welcome receiving submissions from individuals or organisations.
Written evidence received will form the basis for the Sickle Cell Society’s final report, alongside evidence gathered through focus groups and interviews. Some written evidence will be directly quoted in the report. Please explicitly state if any of the submission provided should not be directly quoted or should only be quoted anonymously.
Please submit written evidence to aidan.rylatt@sicklecellsociety.org by Friday 5th May 2023.